Go with the FLOW! How I Scored a Date with A Surgeon.
I FINALLY got lucky and scored a date with a surgeon! The Surgeon’s office called immediately, before the two minutes of tears were dry. It was Wednesday, the day of my diagnosis, and the appointment was set for Friday morning. They were not messing around. I could tell from the speed of mammogram to regram to ultrasound to the ultrasound tech telling me, “I’m calling in the doctor” that there was no time to lose. They told me it would take two days for the results of my biopsy to come in. They called me the next day. What should I wear? Coco Chanel says you should dress like you have a date with destiny. And I do. I grab the Adidas Track pants and disguise how lazy I am with faux fur accessories, including my Wookie apres ski boots.
The month of my mammogram...
Kevin and I entered the surgeon’s office and
instead of being guided to an examination room with your standard paper-covered
table, rolling chairs, hand washing sink and beige cabinets, we were guided into
a conference room, complete with large table about a dozen office chairs, a
projector screen and a pink cupholder in the corner of the table. I bought my own notebook, and they offered me
a pink ribbon pen, but I am refusing to adopt the breast cancer swag because I’m
a party girl who doesn’t want to bring anyone down. Besides, my metal liquid ink pen is classier. I tap it on my red pleather Economist notebook.
The surgeon introduces herself and the nurse that is in the
room. Apparently, you get your own
cancer nurse, too. After the perfunctory
introductions are name and regrets expressed, we dig right into it. She asks me, “What have you read on the
Internet since your diagnosis?”, she asked.
“Nothing.”, I replied immediately.
I know better. I also know the
punchline to WebMD is “You have cancer!”, which I know already. “Good.”, she said, closing her eyes slightly
and with the Mona Lisa smile I will come to know as approval.
“As you know, you had a mammogram on December 26th, then we called
you back for another and ultrasound December 27th, then we performed a biopsy
on January 2nd. The tumor was malignant,
and your diagnosis is invasive ductal carcinoma, which is the most common and
treatable form of breast cancer.” A
large image of my defective breast is projected on the screen. The surgeon continued, “We were looking at
this spot HERE in the mammogram, and HERE in the ultrasound, and we measured it
under 2 centimeters, which is good.”
YEP. It was pretty plain. Pretty defined. Not a black hole like a cyst. There was the pea under the mattress literally
in black and white.
“You might want to take notes.”
I click my superior pen into readiness
“Our recommendation is to do a lumpectomy with lymph node
biopsy. You will meet with a genetic
counselor who will determine whether you are eligible for the BRCA test. If you are eligible, we like to schedule
surgery after we get the test results back in 4-6 weeks, as those might impact
our surgery decision. You will also be
tested for your hormone receptor factors for estrogen and progesterone, as that
will impact your chemotherapy and maintenance drug options. If you test
positive for hormone receptors that is good, because it gives us another
treatment option to cap off those hormone receptors on any cancer cells. Think of a child-proof cap on an electrical
outlet. There is another factor you will
be tested for, Her-2/Neu (she spells it out for me) that if you test positive, that
is not so good and you will need to do chemotherapy. We also recommend radiation, to prevent any
small cells from developing into tumors. This total treatment can take anywhere
from six months to a year, depending on the outcomes of these tests. If you follow our recommendation, we think
your prognosis is very good.”
I am writing this as fast as I can and trying to put this in a
linear fashion from years of being programmed as a project manager. I state to map out the timing and the
milestones. It seems that there are a
few unknown that will impact my cancer project, so I begin to draw a flowchart
with IF/THEN statements.
“Do you have a job?”, the surgeon asks.
“Now I do.”, I quip, hoping to get a glimpse of Mona Lisa’s teeth.
When I had a REAL job
I dig around in my handbag for my lip balm. I thought this was a doctor’s appointment,
not a project planning meeting. I spy my
two most useful tools as a rocker and manual laborer. I pull out my Sharpie and my retractable
blade, slap them on the glossy tabletop and announce, “Let’s DO this! Right here, right now!” The Surgeon is not amused. “Uh, I mean, I’m sure your tools are
BETTER…” Like my pen.
She gives me a pass through the awkward silence, “It’s good to have
a positive attitude through this and I understand you want to get through this
quickly, but there are a lot of factors to take into consideration.”
What stage am I?”, I ask, because everyone keeps asking me.
“We don’t know until the surgery, but here are the criteria for the
stages,“ the surgeon rattles them off and I put them in a linear fashion that
my brain can comprehend:
IF the tumor is under 2 cm, AND there is no cancer in lymph nodes,
THEN you are Stage 1.
IF the tumor is 2-5cm, AND there no cancer in lymph nodes, THEN you
are Stage 2.
IF there is cancer in lymph nodes, THEN go straight to Stage 3, do
not pass GO, do not collect $200.
IF your tumor is over 5 cm AND it’s in your lymph nodes THEN the party’s
over.
She explains the surgical process.
“We take out additional tissue around the tumor, test the periphery, and
if there are malignant cells in the periphery, we may have to go back in and
take more. We test your sentinel lymph
nodes during surgery for malignant cells, and if there is cancer there, we take
more, until we find ones that are clear.
We used to take them all out but we don’t do that anymore. The swelling from the removal of lymph nodes
can be uncomfortable and if you get lymphedema, we can fit you with a
compression sleeve.” My mind goes
immediately to spandex opera-length gloves.
This is getting really complicated.
What happened to having major surgery and going to a house party four
days later, like I did with my hysterectomy? There are more conditional statements to
come. My linear transcription of the
steps starts to become a flowchart. The
fixed items are surgery and radiation.
The timeline now has Genetic testing, the pre-surgery physical, the
radioactive seed implantation and surgery as milestones, but the times are not
set. Everything else is contingent on
the outcome of the decision tree which is now growing branches and leaves, but
is as barren as the lunar surface.
OPTION 1: SURGERY – TIME AND
SCOPE
IF my meeting with the genetic counselor determines I am a good
candidate for the BRCA test, THEN my surgery will be in 6 weeks to allow for
the results.
I want this thing out.
NOW. I’m tapping the metal pen on
the tabletop, indicating my impatience.
“What if I’m NOT a candidate for the test? When can I have my surgery?”, I demand.
IF I am not a candidate for the BRCA test, THEN I can have my
surgery in two weeks.
Why are these people smiling?
TWO WEEKS? Why not
tomorrow? There are more
contingencies. This project has more
milestones inserted into the timeline.
“It will take a couple of days to schedule your genetic
counseling. Then, you have to get a
physical less than one week before your surgery and some blood tests, but no
more than one week out. Then, about
three days before surgery, you will visit radiology. They will insert a radioactive seed, like the
ones used to treat Prostate Cancer, into the tumor. This will guide us to the tumor in surgery
with a Geiger counter, as the tissue does not look different than healthy
tissue.” I start a new page in my
notebook.
The surgeon adds yet another factor into the decision. “You CAN elect to have a mastectomy with one
or both breasts, regardless of the outcome of your genetic counseling. It is your choice. Some people feel better having one or both breasts
removed.”
REALLY? Some people do this
BY CHOICE? You are kidding me. I can’t imagine a scenario where by this
would be a choice unless they were really freaked out or wanted to throw free
cosmetic surgery in there. You would
have to have a gun to my head for either of these. Why didn’t she tell me this in the first
place? That’s kind of a big option to
throw on the table.
“Just for fun, let’s say I choose to have my left breast or both
breasts removed. Does that better my
chances? How does that change my
prognosis?”
“By one percent.”, She closes her eyes slowly and the corners of her
mouth twitch into a knowing smirk.
“One percent.”, I reflexively repeat.
“One percent.”, she affirms.
“We can remove all the tissue, but we never get all of it. There is no guarantee that there isn’t some
tissue left behind that can become cancerous.”
I think about my own experience with breast cancer and the three
people I know whom have DIED from breast cancer. ALL of them had their breasts removed. One was a man. Michele had all the tissue from her ears to
her bellybutton removed. Trace had her
breasts removed, reconstructed and the cancer came back and killed her. “I dinna no ye could git brrreast cancer in
plastic tits!”, she quipped in her Geordie accent. Magoo had all his breast tissue removed ten
years before he died. In a split second,
given all the anecdotal and statistical information, I’m sticking with the
doctor’s recommendation.
OPTION 2: CHEMO OR NO CHEMO
“So if I’m Stage 1, I don’t have to do chemo?” I get the not-so-fast-lady look and she
explains. “If you are Her-2/Neu positive, THEN you have to do chemo.”
“There’s no way out of it? Do
I have to do the chemo?” I am clearly in
the bargaining stage.
“Yes, there’s really no way around it. If you are Her-2/Neu positive, you really
need to do that particular chemo, Which the course of treatment is one
year.”
Sounds like Her-2/Neu Positive is something you DON’T want to
be. I’ve already decided I’m not positive. There is no way I can do chemo for a
year. That would turn me into a party
pooper. I picture myself wheeling a
crystal-studded IV bag around wherever I go.
This decision is not up to me.
I don’t like that one bit. IF
there is no cancer in my lymph nodes, AND I am Her-2/Neu negative THEN I do not
have to do chemo. This is the scenario I
lay out in my notebook.
OPTION 3: HORMONE
RECEPTORS
I had heard the term “triple positive” and “triple negative”
thrown around here and there with cancer and I heard triple negative was BAD,
which seemed to me counter-intuitive.
Testing positive for breast cancer was BAD. Most tests with a negative result are GOOD. My friend Michele was triple negative, and
someone told me this was bad. I have no
idea what I am. Given I’m over an hour
into this meeting and there’s still a ways to go.
“So, I’ve heard the terms triple positive and triple
negative thrown out there. How do I know
what I am and what does that mean?” I
have the feeling I’m about to feel kinda stupid with what the answer is.
The surgeon does her Mona Lisa smile again with closing and
opening of eyes slowly. “We will not
know that until later. We test you for
your hormone receptors. Think of the
cancer like an open outlet. If you test
positive for the progesterone and estrogen receptors, then we use medication to
block those receptors so the hormones cannot affect the cancer cells. Think of a child-proof cover for the plug.”
“Why is it triple positive or negative? What is the third factor?”, I must have
missed something.
“That’s the Her-2 factor we discussed before.”, she says.
“So what happens if I’m hormone receptor negative?” I get my pen ready.
“That just means the maintenance pills are not a treatment
option, that we can’t block those receptors.”
That doesn’t sound good.
I am confused. Being
triple negative is bad, but being Her-2 negative is good. I thought you are all one or all the
other. I am mulling this over. The triple test is putting a fork in the fork
of my flow chart. My flow chart is
looking pretty messy by now.
Getting back to the project at hand, I go back to building
out the timeline. “How long will all
this take?”
The surgeon continues with more IF/THEN conditions for the
flow chart. “IF you do NOT have cancer
in your lymph nodes AND you are not Her-2 positive, your treatment will be
about 6 months from start to finish. IF
you are Her-2 positive, THEN that course of treatment is one year.”
Trying to make sense of all this
“So how does this process go from start to finish?”, I
ask. I have a project plan to complete.
Some of these conditions are fixed. The difference in where I wind up at the end
of the flow or how much time it will take are vastly different. Here’s what I have in my notebook, and will
have to make this a tidier chart when I get home:
Step 1: Appointment
with Genetic Counselor. IF YES to BRCA
test, surgery in 6 weeks. If NO, surgery
in two weeks.
Step 2: Appointment
for Pre-op Physical and blood test one week before surgery. IF NO to Step 1, then physical in a week but
no more than a week before surgery. The
step is fixed, the timing is not.
Step 3: Appointment
for radioactive seed no more than 3 days before surgery. They implant a radioactive seed so the surgeon
can find the tumor with a Geiger counter.
Contrary to popular belief, this cancer is not the black mass it is on
the screen and is not visible to the naked eye.
Step 4: Schedule Surgery
in six weeks, IF there is no BRCA test.
Step 5: Schedule
appointment with Radiologist. Radiation
is fixed, but timing comes after surgery.
Step 6: IF I am Her-2
positive AND/OR I have cancer in my lymph nodes THEN I will have to schedule an
appointment with the oncologist.
Step 7: IF I am
hormone receptor positive, THEN I go on maintenance pills for five year. IF not, OH WELL, but that’s not good.
I can’t imagine keeping track of all these
appointments. Guess what? I don’t have to! They explain that helpful cancer nurse comes
with a cancer secretary who makes all of these appointments for me. IF one appointment moves, THEN cancer
scheduler moves all the other appointments.
They guide me to the desk of the scheduler, and I’m anxious to start
this project ASAP.
First Day of Work Orientation Packet
“Can I talk to the genetic counselor TODAY?”, I ask. It’s Friday afternoon, and I hate waiting the
weekend and being a slave to the 9-to-fivers.
She assures me she will place the call today, and if they do not call
me, she gives me the number to call.
It’s January 5th.
I scheduled my surgery for Valentine’s Day. I hate the holiday anyway, and you can’t get
a reservation anywhere good so screw it.
If I have to get my tits cut off, so be it. I think it’s actually kind of brilliant. Why not have surgery on valentine’s day? I’m going to get flowers and candy for having
surgery. I certainly don’t require them
on any other February 14th.
So there it is, all mapped out. The cascading appointments of my
project. It’s like planning a party or a
show. First you get the date and then
the venue, then you schedule the DJ and/or the bands, arrange for the food and
drink, make the flyers and promote it at least a few weeks before the show,
send out reminders, arrange for the gear and all the technical stuff, then it’s
all over in a few hours, and you recuperate.
None of this is in my control, except pushing the timeline
if I can. I’m determined to get through
this as fast as possible, but understand I have to go with the flow. I can’t impact much except to educate myself on all this. All I want to do is crawl back
in bed. Kevin and I get some lunch and
you could hear the gears turning in our silence. I've had dates took less time than this meeting at two and a half hours. I went home and drew my flowchart, but it looks like I have my work cut out for me.





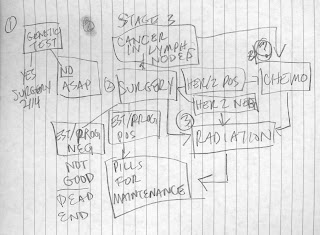



I know this had to be a bitch to write. I'm glad you stood up to the challenge. When you drew a flowchart for me (yes, I have my own personal Lindsey handwritten flowchart) I said, "I totally get it now! You need to take the flowchart public." The info in this is personal and insightful and user friendly. It's missing the size piece (not THAT size-people get your heads out of the toilet). My understanding was the size and your superpower assessment of the BRCA test determined the rest. Am I jumping the narrative arc? If so, sorry. I hate that you have cancer, I hate what you're going through, and yet I am so very proud of how you're going through it. One more thing, you understand that this is a teachable moment. Thank you for being such a cool teacher. xxxx.
ReplyDelete